Flat Foot Deformity
What is Flatfoot deformity?
Flat foot deformity is now known as Progressive collapsing foot deformity (PCFD), previously known as adult-acquired flatfoot deformity (AAFD) or more classically posterior tibial tendon dysfunction (PTTD). It is a complex pathology defined by the collapse of the instep - medial longitudinal arch, outward deviation of the heel - hind foot valgus deformity. Forefoot abduction - toes deviated out, forefoot supination - great toe metatarsal bone elevated. Valgus deformity of the ankle - inner loosening and outer collapse of the ankle joint may develop in the later stages of the process. Each component of the deformity can commence as flexible and progress to rigid and may lead to arthritis of affected joints. (1)
How common is the flatfoot deformity?
The Flat foot deformity is reasonably common and may progress depending on ethnicity, gender, Body Mass Index, associated medical conditions. The prevalence of plano-valgus deformity among non-Hispanic whites was reported to be 17% and greater among African Americans at a rate of 34% in a 2003 study by Dunn et al. (2) Women are more commonly affected than men, and the median age of presentation is 55 years (3). Obesity, hypertension, diabetes, hyperlipidaemia, genetic predisposition and high impact sports have been identified as contributors to the development of the pathology (1). Up to 76% of patients with PCFD have associated tight gastrocnemius muscle or Achilles tendon (4).
What causes this deformity to develop?
The posterior tibial tendon degeneration elongation and weakening was traditionally thought to be a key pathophysiological component in the development of PTTD following a landmark paper by Johnson and Strom in 1989 (5). Later studies has shown that spring ligament (ligament connecting inner heel bone and navicular bone, functioning like a hammock for the head of the talus - ankle bone) weakening and elongation allows peritalar subluxation (navicular bone moves up and out over the head of the talus and heel bone moves to the outer side from under the talus. Talar bone in turn rotates in and points down, potentially initiating the deformity before posterior tibial tendon is subjected to overload. (6) Plantar fascia elongation is another factor of PCFD development. Deltoid ligament complex is often elongated as a result of prolonged strain in the case of chronic planovalgus deformity. Acute deltoid ligament ruptures involving spring ligament and tibionavicular ligament as in Hintermann type 3 can also result in PCFD. In such a case a realignment procedure should be combined with the deltoid ligament repair. (7)
What are the patients complaining off?
Most patients with PCFD will complain of - medial ankle and foot pain (pain in the inner instep) in the early stages of the disease. Later stages may involve lateral pain due to subfibular impingement. Peroneal tendon (Outer ankle tendons), get trapped between the heel bone and the tip of the fibular bone). (1)
What are the nonoperative treatment options?
Initial treatment involves medial arch supporting orthoses (Insoles), physiotherapy focused on gastrocnemius muscle and achilles tendon stretching, PTT eccentric strengthening, weight-loss (8,9). Surgery is commonly considered if no improvement was achieved with 6 months of nonoperative treatment.
What are the surgical treatment options for early stage flat foot deformity?
Medialising Calcaneal Osteotomy and Flexor Digitorum Longus tendon transfer is a traditional procedure for flexible Johnson Strom stage 2A deformity with good or even excellent reported outcomes in mid and long term cases series (10,11). Concerns remain regarding low correction potential, lack of medial longitudinal arch reconstitution, no improvement of forefoot abduction with the original technique.
Spring ligament repair has been practised, however the ligament is too degenerate for a reliable primary repair and fails early with forefoot abduction and during weight-bearing. Spring ligament augmentation with a suture tape has been described by Acevedo and Vora (12). Pasapula et al has shown significantly superior resistance to forefoot lateralisation with spring ligament augmentation with suture tape in comparison to repair alone in cadaveric specimen study. (13) Fogleman et al. has consecutively reported average of 62 weeks follow up outcomes of 57 consecutive patients who had flatfoot reconstruction including Spring ligament suture tape augmentation. Significant improvements were seen in the radiographic parameters evaluated. Five patients had subsequent operations including one deep infection, 2 hardware removals remote to the spring ligament augmentation, 1 ankle arthrodesis, and 1 triple arthrodesis. (14)
Mr. Chlebinskas performs Minimally Invasive Medialising Calcaneal Osteotomy (MIMCO), where the rear side of the heel bone is cut using a percutaneous slow spinning, high torque burr. The hind part is then shifted inwards about 10-12mm and fixed in new position using large headless compression screws via small incision. Achilles tendon requires percutaneous lengthening Hoke procedure more often than not.
Mr Chlebinskas has developed, described and published a minimally invasive procedure, employing an arthroscope to address the weakened spring ligament and deficient posterior tibial tendon. Arthroscope is employed to harvest FDL tendon. Via percutaneous incisions synthetic internal brace is used to reconstruct the spring ligament that serves as a hammock for the talar head. Once the hammock is tightened - the head of the talus will return to it's neutral position. FDL - lesser toes flexing muscle tendon is transferred and fixed into the navicular bone to reinforce the construct and boost the power of PTT. This procedure certainly may reduce the risk of wound complications. You can read about it and watch the video in the scientific paper, by clicking on this link. You can also watch the short video of it here.
What is the procedure suitable for more advanced stage flatfoot deformity?
Tripple fusion is the procedure where the joints about the talus: talonavicular joint, subtalar joint and calcaneocuboid joint are denuded of cartilage, restored to normal anatomical alignment and secured with screws or plates in order for the bones to fuse.
Mr. Chlebinskas performs this procedure via percutaneous inions with a use of the arthroscope to prepare the joints denuding the remnants of the cartilage and securing the aligned bones with headless compression screws to achieve fusion. Achilles tendon lengthening is almost universally performed as a part of this procedure.
Such procedure allows restored alignment, but leaves the hindfoot rigid. It is reserved for rigid and arthritis associate flatfoot deformity. Also for elderly, low demand or very high BMI.
What is the post operative regime following :
2 weeks no weight bearing and immobilisation in a Back slab.
2 weeks elevation at the heart level 23hr a day.
At 2 weeks follow up appointment the wound check is performed.
At 2 weeks follow up appointment waking boot is applied and touch weight bearing is allowed. Usually two crutches or a walker frame are required for 4 weeks.
At 6 weeks follow up appointment X-Rays are obtained.
At 6 weeks weight bearing as pain allows weaning off the walking aid can be commenced with a walking boot.
From 6 weeks after surgery gradual return to physical activities are advised. Starting with walking, cycling,
At 10-12 weeks follow up appointment X- Rays are obtained
Walking with regular shoes and medial arch supporting semi rigid insole can be commenced.
It is not recommended to drive a car for 10 weeks after surgery. (You can drive automatic gear box car 2 weeks after surgery if your left foot was operated).
Possible risks and complications:
Intraoperative
Nerve or vessel damage (numbness, pins and needles or bleeding, necrosis)
Anaesthetic risks
Early postoperative
Swelling, bruising, pain
Surgical site infection (superficial wound infection or deep bone infection - osteomyelitis)
Thrombosis (DVT and/or PE)
Late postoperative
Recurrence - often some of the achieved correction is lost, but pain seldom comes back.
Nonunion (fusion site doesn’t heal)
Maluinion (bone heals in undesired position)
Complex regional pain syndrome (Sensitive, swollen, atrophic foot) 0,4%
Metalwork failure (screws break, migrate, or irritate tissues)
Adjacent joint arthritis - subtalar, talonavicular joints may wear in 10-20 years from surgery
Need for further surgery.
List is extensive but likelihood of these risks is small.
How to prepare for the surgery
Preoperative period
Have WEIGHT BEARING x-ray radiograms. Lateral of the foot and ankle, AP of the ankle, dorsoplantar view of the foot, hindfoot alignment view.
MRI scan is not mandatory, but helps to asses spring ligament attenuation and PTT degeneration.
Blood tests including Full Blood Count, Coagulation screen, Urea & Electrolytes, VitD not older than 1 month;
Tell the doctor if you have diabetes and if so have HbA1c not older than 1 month.
Tell the doctor if you are using blood thinning medication
You can use Aspirin throughout the procedure for cardiological reasons.
Don’t use nicotine 6 weeks before and 6 weeks after surgery. This includes cigarettes, cigars, vape with nicotine etc. This will reduce the risk of
Thrombosis (DVT and PE),
The risk of infection by 2.04 times
The risk of nonunion by 2.5 times
Use Vit D (1000IU) and Calcium (500mg) supplement 6 weeks prior and 6 weeks after the surgery.
Use high dose Vit C (500-1000mg) 6weeks before and 6 weeks after the surgery This will reduce the risk of CRPS.
Dont use Non steroidal anti-inflammatory drugs NSAIDs Before and 6 weeks after surgery.
On the day of surgery
Don't eat 8 hr before surgery
You can drink plain water up to 2hr prior to surgery
Take your medication that you use regularly on the morning of surgery.
Knapp PW, Constant D. Posterior Tibial Tendon Dysfunction. [Updated 2024 May 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542160/
Dunn JE, Link CL, Felson DT, Crincoli MG, Keysor JJ, McKinlay JB. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol. 2004;159(5):491-498. doi:10.1093/aje/kwh0711.
Deland JT. Adult-acquired flatfoot deformity. J Am Acad Orthop Surg. 2008;16(7):399-406. doi:10.5435/00124635-200807000-00005
Mohamed, Sara & ALanni, Enas & Faggal, Mona & Ibrahim, Mona. (2022). Prevalence of Calf muscle tightness in asymptomatic flat foot subjects. Egyptian Journal of Physical Therapy. 10. 26-31. 10.21608/ejpt.2021.71608.1038.
Johnson, K. A., & Strom, D. E. (1989). Tibialis posterior tendon dysfunction. Clinical Orthopaedics and Related Research (1976-2007), 239, 196-206.
Pasapula, Chandra & Cutts, Steven. (2017). Modern Theory of the Development of Adult Acquired Flat Foot and an Updated Spring Ligament Classification System. Clinical Research on Foot & Ankle. 05. 10.4172/2329-910X.1000247.
Hintermann B, Valderrabano V, Boss A, Trouillier HH, Dick W. Medial Ankle Instability: An Exploratory, Prospective Study of Fifty-Two Cases. The American Journal of Sports Medicine. 2004;32(1):183-190. doi:10.1177/0095399703258789
Ross MH, Smith MD, Mellor R, Vicenzino B. Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport Exerc Med. 2018;4(1):e000430. Published 2018 Sep 19. doi:10.1136/bmjsem-2018-000430
Karthika, N & Kumar, R & Kumar, R.V. & Vasanthan,. (2022). Efficacy of Tibialis Posterior Strengthening Exercise with Obesity Reduction Program in Flexible Flatfoot among Obese School Children. Indian Journal of Physiotherapy & Occupational Therapy - An International Journal. 16. 120-127. 10.37506/ijpot.v16i2.18043.
Myerson MS, Badekas A, Schon LC. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004;25(7):445-450. doi:10.1177/107110070402500701
Acevedo J, Vora A. Anatomical reconstruction of the spring ligament complex: "internal brace" augmentation. Foot Ankle Spec. 2013;6(6):441-445. doi:10.1177/1938640013499404
Pasapula C, Devany A, Fischer NC, et al. The resistance to failure of spring ligament reconstruction. Foot (Edinb). 2017;33:29-34. doi:10.1016/j.foot.2017.05.006
Fogleman JA, Kreulen CD, Sarcon AK, Michelier PV, Giza E, Doty JF. Augmented Spring Ligament Repair in Pes Planovalgus Reconstruction. J Foot Ankle Surg. 2021;60(6):1212-1216. doi:10.1053/j.jfas.2021.05.010
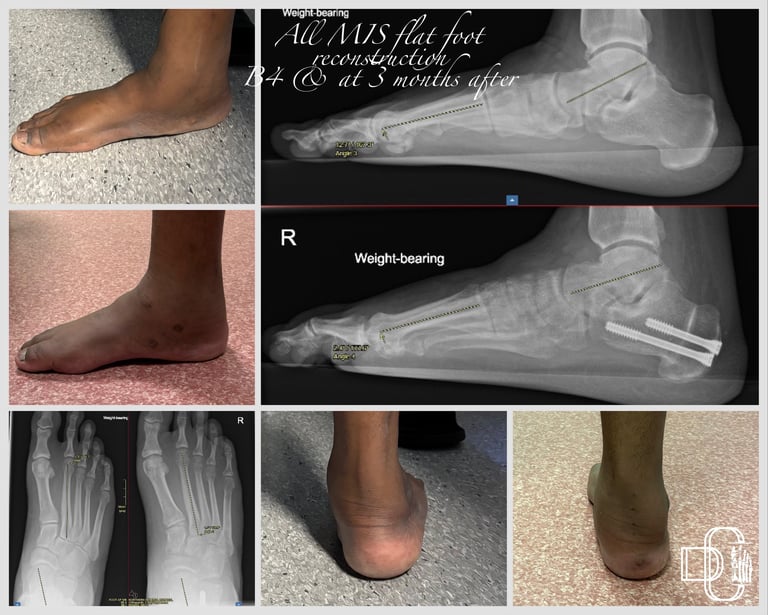
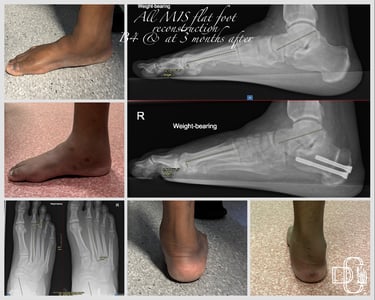
Treatment with Minimally Invasive Medialising Calcaneal Osteotomy MIMCO, Internal brace and FDL transfer