Insertional Achilles tendinopathy
What is Insertional Achilles Tendinopathy and Haglund's deformity?
Insertional Achilles tendinopathy and Haglund’s deformity is a condition affecting the rear part of the heel bone, presenting with a painful thickening of the lowest part of the Achilles tendon, a sore lump, difficulty wearing shoes and performing physical activities.
How does Insertional Achilles tendinopathy and Haglund’s deformity develop? (Išskleidžiamas)
It is now believed that with longer upper end of the heel bone, the contact between upper rear corner and the insertional part of the tendon is causing repetitive micro damage. In the long run degeneration develops:
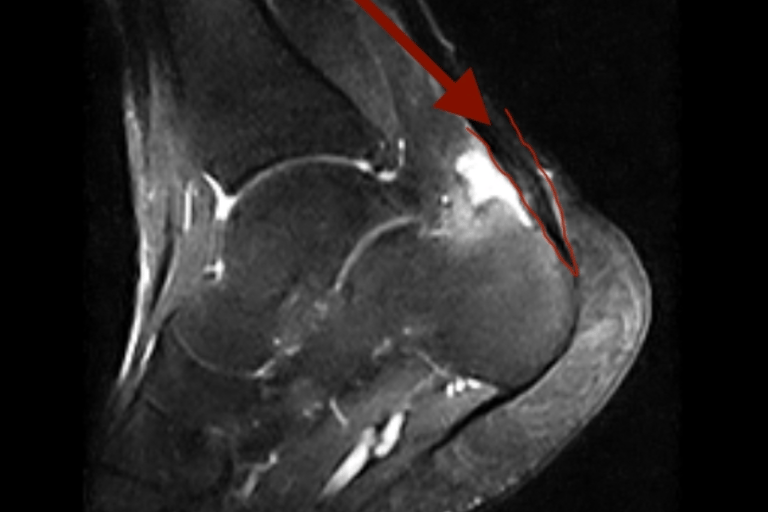
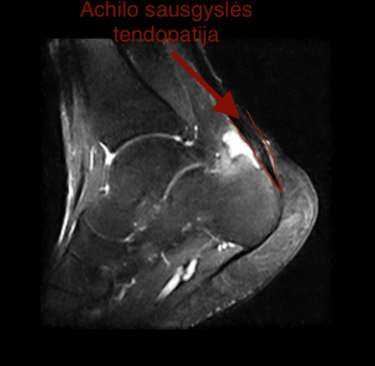
Tendinopathy - Achilles tendon becomes thickened and painful secondary to fat, abnormal collagen, calcium, new vessels and nerves deposits.
Treatment with Zadek osteotomy

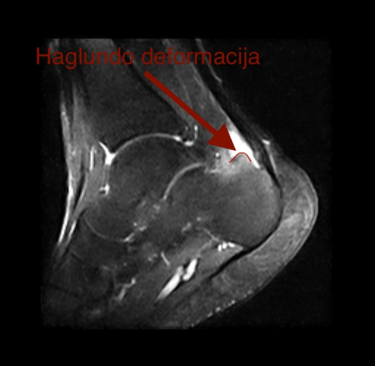
The complex of all these changes is called Haglund’s syndrome. The patient complains of the painful lump, difficulty finding appropriate shoe-wear, resuming physical activities.
Non Operative treatment
Non operative treatment is limited and often provides only temporary relief.
Pain killers, icing, activity modification often provides only temporary relief
Physiotherapy with Excentric strengthening protocols is effective in up to 30% (1).
Silicone heel cups may relieve symptoms temporarily, but will shorten Achilles tendon and worsen the process in the long run.
Appropriate shoe-wear with soft heel cup or slippers, prevent painful rubbing.
Extracorporeal shock wave therapy is more effective for the treatment of Non insertional Achilles tendinopathy. (2)
Ultrasound guided Steroid injection can increase the risk of tendon rupture.
PRP - Platelet Rich Plasma injection effectiveness for IAT or NIAT is not proven. (3)
Operative treatment
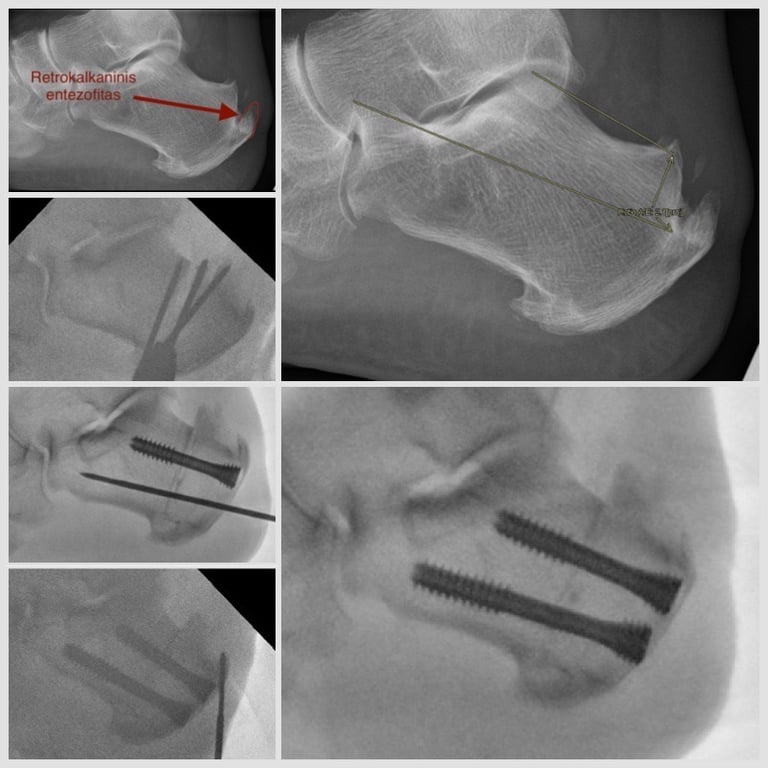
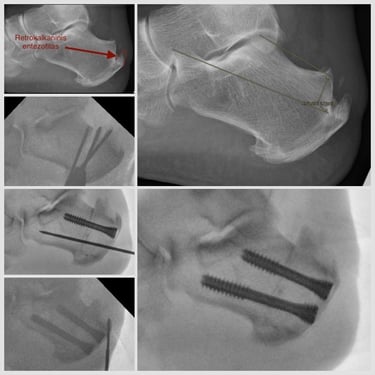
Mr. Donatas Chlebinskas offers percutaneous Zadek Dorsal Closing Wedge Calcaneal Osteotomy (DCWCO) for the management of IAT. Procedure is performed on the day surgery basis, usually under general anaesthetic. Percutaneous 4-6mm incisions are used. Bone cuts are performed under x-ray control using slow spinning high torque Shannon burrs and Wedge burrs. The wedge of bone is taken out based at the top of the rear heel bone. Once closed and fixed rigidly with special screws - fixation is strong
enough o permit weight bearing from day one, but back slab is applied and non weight bearing regime is advised for first 2 weeks. This operation assures the following affects:
Haglund deformity bone spur is moved away from the achilles tendon, decreasing the impingement.
Achilles tendon insertion point is raised higher therefore decreasing the tension on the tendon.
Rarely the operation can be combined with rear ankle keyhole procedure called posterior ankle arthroscopy to remove the retrocalcaneal bursa and shave the remaining bone spur.
Why should you choose percutaneous Zadek osteotomy over standard open procedure?
Small percutaneous incisions reduces the risk of infection and wound complications, which is quite high in open surgeries because of poor blood supply to the region.
Zadek osteotomy does not involve detaching and reattaching Achilles tendon as the standard open surgery. Therefore Achilles tendon rupture risk is reduced.
Less postoperative pain. Lower analgesic requirements.
Ankle is kept in neutral rather than en pointe position and weight bearing is permitted 2 weeks after surgery as pain allows.
Lowe risk of Thrombosis as DVT and PE.
This surgery is suitable for profesional athlets and permits return to competitive athletic activities at 21 weeks in open surgery. (3) This will be reduced by percutaneous procedure.
What is the post operative regime for the best outcomes:
2 weeks using a Back slab.
2 weeks elevation at the heart level 23hr a day.
At 2 weeks follow up appointment the wound check is performed.
At 2 weeks follow up appointment waking boot is applied and weight bearing is permitted as pain allows. Usually waling with two crutches for 2 weeks and one crutch in the opposite hand for further two weeks is required.
At 6 weeks follow up appointment X-Rays are obtained.
At 6 weeks appointment regular comfortable footwear is commenced.
From 6 weeks after surgery gradual return to physical activities are advised. Starting with walking, cycling, swimming, transitioning to jogging at 10-12 weeks after surgery.
It is not recommended to drive a car 6 weeks after surgery. (You can drive automatic gear box car 2 weeks after surgery if your left foot was operated).
Possible risks and complications:
Intraoperative
Nerve or vessel damage (numbness pins and needles or bleeding, necrosis)
Achilles tendon damage
Incomplete resolution of the lump
Calcaneocuboid joint damage
Anaesthetic risks
Early postoperative
Swelling, bruising, pain
Surgical site infection (superficial wound infection or osteomyelitis)
Thrombosis (DVT and/or PE)
Late postoperative
Plantar fasciopathy - pain at the bottom of the heel
Recurrence (deformity comes back).
Nonunion (bone cut doesn’t heal) Pseudoartozė (Kaulinis nesugijimas),
Maluinion (bone heals in undesired position)
Hypertrophy of the scar (sensitive big scar).
Complex regional pain syndrome (Sensitive, swollen, atrophic foot) 0,4%
Metalwork failure (screws break, migrate, or irritate tissues)
Need for further surgery.
List is extensive but likelihood of these risks is extremely small. Most of them only theoretical and not reported in the literature.
How to prepare for the surgery
Preoperative period
Have WEIGHT BEARING x-ray radiograms. Lateral of the foot and ankle and AP of the ankle and dorsoplantar view of the foot.
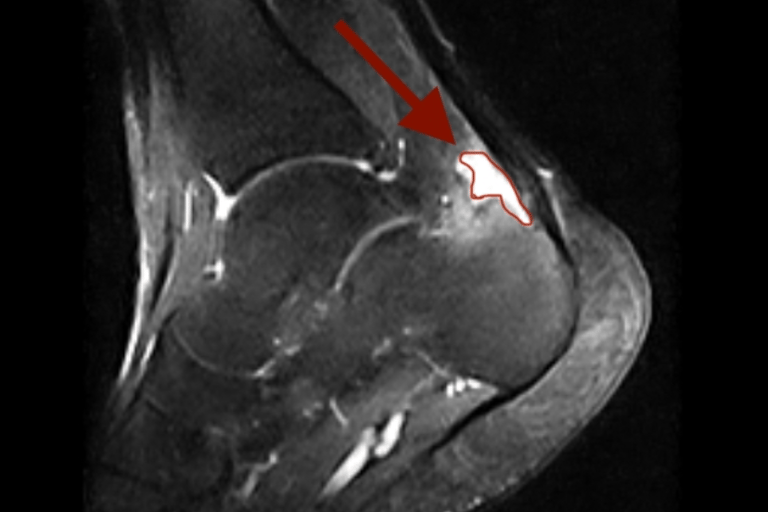
MRI scan is not mandatory, but helps to better plan surgery and differentiate from other potential problems that may present with similar symptoms.
Blood tests including Full Blood Count, Coagulation screen, Urea & Electrolytes, VitD not older than 1 month;
Tell the doctor if you have diabetes and if so have HbA1c not older than 1 month.
Tell the doctor if you are using blood thinning medication
You can use Aspirin throughout the procedure for cardiological reasons.
Don’t use nicotine 6 weeks before and 6 weeks after surgery. This includes cigarettes, cigars, vape with nicotine etc. This will reduce the risk of
Thrombosis (DVT and PE),
The risk of infection by 2.04 times
The risk of nonunion by 2.5 times
Use Vit D (1000IU) and Calcium (500mg) supplement 6 weeks prior and 6 weeks after the surgery.
Use high dose Vit C (500-1000mg) 6weeks before and 6 weeks after the surgery This will reduce the risk of CRPS.
Dont use Non steroidal anti-inflammatory drugs NSAIDs Before and 6 weeks after surgery.
On the day of surgery
Dont eat 8 hr before surgery
You can drink clear water up to 3hr prior to surgery
Take your medication that you use regularly on the morning of surgery.
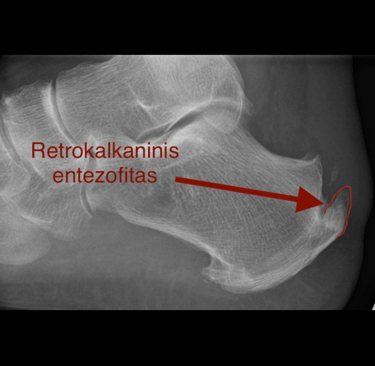
Retrocalcaneal bursitis - inflammation of the fluid sack between the Achilles tendon and the heel bone.
Haglund’s deformity - The bone spur progressively enlarges at the rear upper end of the heel bone.
Retrocalcaneal Enthesofite - additional spur forms behind Achilles tendon insertion point.