Hallux Rigidus
What is Hallux Limitus and Hallux Rigidus?
Metatarsophalangeal joint is at the base of the great toe. Hallux limitus - is a condition characterized by pain and limited motion of this joint and can be seen as early arthritis. It may progress to Hallux Rigidus - a condition where the joint looses most of the motion.
What is the initial treatment?
Initial treatment involves rigid insoles, rigid sole shoes, steroid injection, pain killers and activity modification. With failed non operative treatment for at least 3 months, surgery can be considered.
What are the surgical options for Hallux Rigidus?
When nonoperative treatments for Hallux rigidus has been exhausted, surgical procedures are discussed. They range from cheilectomy, decompression osteotomy to fusion.
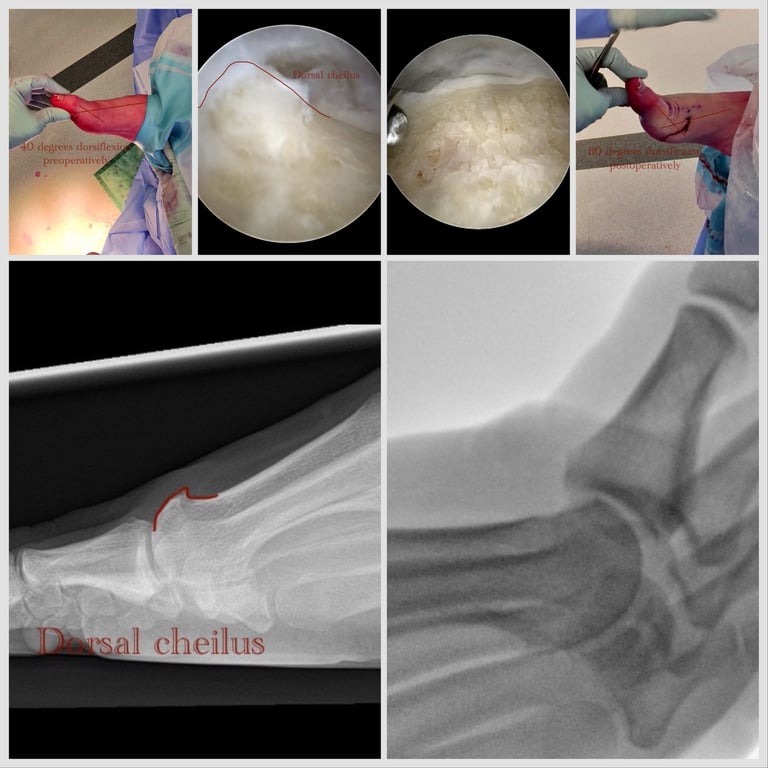
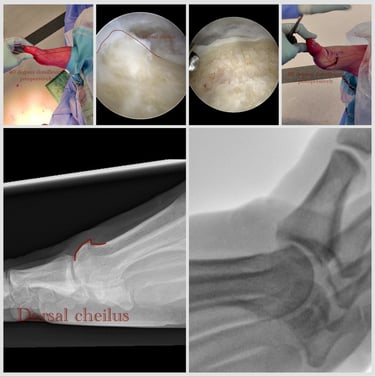
Dorsal Cheilectomy
Dorsal cheilectomy is a procedure where the bony prominence of the metatarsal head and base of the phalanx is surgically removed to allow greater and less painful movement
It can be performed as open procedure but percutaneous and arthroscopic procedure has Advantages over open:
- small incision
- less postoperative pain
- quicker wound healing
- shoes can be worn 7-10 days after surgery
- x8 maginified view allows quality assessment of the joint and precision procedure
Procedures that can be performed concomitantly:
debridement - loose cartilage flaps, excess of scar tissue removed with special instrument called dissector, shaving and sucking debris out at the same time
Microfractures: bone found under damaged cartilage is perforated with sharp surgical owl in order for it to bleed and form scar like tissue called fibrocartilage
A study published by Hickey et all in the European Journal of Orthopaedic surgery and Traumatology in 2020, reported 4 year outcomes of 36 patients following MIS arthroscopic cheilectomy.
Thirty patients (83%) reported they would recommend the procedure.
Mean postoperative improvement in pain was 69% (range 0-100).
Twenty-seven (84%) of patients reported either no pain (28%) or mild pain (56%).
For patients who reported any pain, the mean pain experienced was rated as 3.4 out of 10 (range 1-9).
Twenty-nine (81%) patients reported they could wear a 'fashionable' shoe postoperatively.
Risks of this procedure are relatively very low and include:
Infection,
nerve damage that may result in partially numb toe,
tendon damage that may result in drooping toe,
ongoing arthritis (progressing pain and stiffness),
need for further surgery often in the form of decomperrive osteotomy, or fusion.
Aftercare:
surgical shoe is worn 7-14 days
weight bearing as tolerated is allowed immediately after surgery
elevation to heart level 23hr a day is recommended for 1 week
movement of the toe by hand or actively is commenced as soon as pain allows - 3-5 days after surgery
return to light sports like cycling and swimming after 2 weeks
return to jogging at 6 weeks
return to contact or team sports at 12 weeks
full recovery is about 6 months, but can last up to 12 months
Percutaneous Treatment
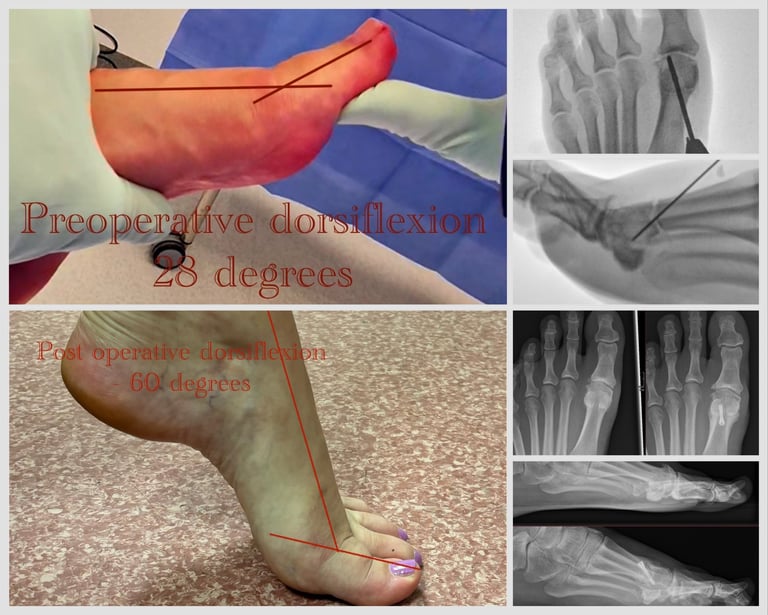



Decompression osteotomy
Decompression osteotomy - is a procedure that is recommended for more advanced arthritis as Coughlin Shurnas stage 2-4. It is also suitable for patients with longer or elevated first metatarsal and In younger patients with advanced arthritis wishing to preserve motion and avoid fusion.
Equivalent to above described cheilectomy procedure is performed percutaneously. At the end of the procedure, shortening decompressive chevron shaped osteotomy is performed at the level of the metatarsal neck and secured with a headless compression screw.
H Davies et al. Has published A comparison of minimally invasive dorsal cheilectomy and dorsal closing wedge osteotomy in the treatment of hallux rigidus.”in a journal or Foot Ankle Surg. 2022
The authors retrospectively compared groups of 38 treated with cheilectomy and 37 with Youngswick like osteotomy and concluded that both significantly improve pain and function in patients with mild-to-moderate hallux rigidus. However, the osteotomy group showed superior functional outcomes, suggesting that joint decompression through shortening and plantarflexion provides additional benefit over cheilectomy alone."
Complication profile is similar to cheilectomy, however additional low risk of hardware irritation, hardware migration, nonunion.
Importantly, the osteotomy is low risk procedure in comparison to resurfacing and joint replacing procedures and allows easier fusion procedure in case of future progression of arthritis.
Aftercare:
surgical shoe is worn for 6 weeks
weight bearing as tolerated is allowed immediately after surgery
elevation to heart level 23hr a day is recommended for 1 week
movement of the toe by hand or actively is commenced at 2 weeks after surgery
return to light sports like cycling and swimming after 6 weeks
return to jogging at 12 weeks
return to contact or team sports at 16 weeks
full recovery is about 6 months, but can last up to 12 months
Metatarsophalangeal joint arthrodesis
MTPJ arthrodesis is a fusion procedure where severely painful and stiff joint is surgically closed by removing residual cartilage and placing hardware in functional position allowing it to unite as one bone. The adjacent joints like interphalangeal and tarsometatarsal joint re functions and maintain the function, permitting standard activities of daily living and even athletic activities.
Cycling, hiking, tennis, golf and even short distance running is possible after having MTPJ arthrodesis.
Percutaneous procedure is possible, however recommended for patients with good bone stock and absence of deformity. Plate fixation arthrodesis is recommended for inflammatory arthritis, bunion associated arthritis and osteoporotic bone.
Additional risks include nonunion, metalwork irritation, adjacent joint arthritis.