Mr. Donatas Chlebinskas MD, FEBOT, FRCS Orth






Hallux Valgus - Bunion
What is Hallux valgus?
Hallux Valgus or bunion is one of the most common deformities of the foot. More than 23% of adults younger than 65 years old and more than 35% of older than 65 year olds have a bunion deformity. Ladies are more likely to get a bunion than men. However not all the deformities will cause problems. (1)
How does a Hallux Valgus deformity develop?
A mixture of factors as age, hyper-laxity (having overly mobile joints), family history and some environmental factors as wearing high heel shoes plays a role in developing Hallux Valgus. Ligaments and capsule supporting the joint at the base of the great toe stretches, lengthens and becomes unsupportive. Bone short of great toe called first metatarsal (M1) deviates inward, great toe itself deviates out. Toe rotates inward, muscles and tendons passing along the foot becomes a deforming force that worsens the deformity. Forefoot widens, shoes become too narrow and rub over the metatarsal (M1) head, causing it to inflame. Painful bunion develops. As deformity worsens 2nd toe assumes adaptive hammertoe deformity, which causes callosity over the back of the toe. 2nd metatarsal (M2) becomes proud at the sole of the foot and causes painful callosity known as metatarsalgia. Further worsening of the deformity causes over-crossing of the 2nd toe over the great toe often associated with sores between the toes. Regular shoes becomes too narrow or even too painful to wear and wears out too quickly.
What are the Treatment options?
Conservative measures as night splints, braces or spacers for Hallux Valgus are often ineffective, may slow but does not stop deformity progression and sometimes may exacerbate symptoms by rubbing over the painful bunion (2).
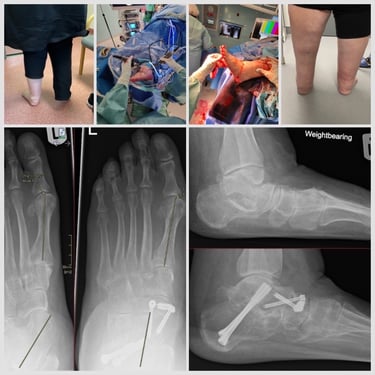
The most reliable solution is surgical treatment. After careful assessment and studying the X-Rays of your foot the most suitable treatment for your bunion can be determined. Most often it is MICA (minimally invasive Chevron and Akin). This surgical procedure is suitable for mild to severe bunions with rare exceptions (3).
MICA is carried out via few 4-6mm surgical stab incisions. Bony cuts are performed using special bone cutting burrs called Shanon burrs, spinning at low repetition but high torque. Constant water flow irrigates site of surgical cuts and prevents harmful bone overheating. Deformity correction and fixation with special beveled positional screws is performed Under X-Ray control. Fixation is strong, permitting weight bearing through operated leg using surgical stiff sole shoe on the same day.
Why should you choose minimally invasive bunion correction MICA over standard open surgery like Scarf and Akin?
Small percutaneous incisions provides better cosmetic result
Less post operative pain with less required analgesics.
Better preserved range of motion
Operation is performed without violating the capsule of the MTP joint, with rare exceptions.
More versatile correction: M1 head rotation and distal metatarsal articular angle are corrected.
Suitable for severe deformities
Lower risk of recurrence (4)
What should you do postoperatively to achieve the best results?
Keep operated leg elevated for 23hr a day for the first 2 weeks.
Bandages are removed and wounds are checked during the post operative visit at 2 weeks.
Special surgical shoe is used for 6 weeks. Full weight bearing with the shoe is permitted.
You can wear rigid sole trainers from 6 weeks after surgery.
Crutches are usually unnecessary with rare exceptions.
Check X-Rays are performed 6 weeks after surgery including side and front views of the foot.
Physical activities are gradually recommenced from 6 weeks after surgery.
It is not recommended to drive for 6 weeks after surgery. A car with an automatic gear box can be driven a day after surgery if the left foot was operated.
What are the possible risks and complications?
Intraoperative
Bone fracture
Varus deformity (hypercorection)
Nerve, vessel or tendon damage would cause numbness, bleeding or dysfunction respectively
Great toe shortening
Anaesthetic complications
Early complications
Swelling, bruising, pain, bleeding
Infections (Surgical Site infection SSI; Deep infection - osteomyelitis)
Clot in the vein - Deep vein thrombosis (DVT), Pulmonary embolism (PE)
Late complications
Recurrence about 7.7% (4).
Avascular necrosis AVN - first metatarsal head bone infarct
Nonunion
Malunion
Stiffness of the first metatarsophalangeal (MTP) joint
First MTP joint arthritis.
Metatarsalgija (pain in the sole of the forefoot)
Scar hypertrophy - hard painful scar
Complex regional pain syndrome (CRPS) - self limiting increased sensitivity, swelling, atrophy globally in the foot - 0,4%
Screw migration, fracture, tissue irritation
Need for further surgery
Even though the possible risks list is extensive, the rates of those risks are extremely rare and most of the risks are not reported in the published case series at all.
How to prepare for the surgery?
Preoperative period
Have WEIGHT BEARING x-ray radiograms of the foot in the lateral and dorsoplantar planes available for the first appointment.
Blood tests including Full Blood Count, Coagulation screen, Urea & Electrolytes, VitD not older than 1 month;
Tell the doctor if you are using blood thinning medication
You can use Aspirin throughout the procedure for cardiological reasons.
Don’t use nicotine 6 weeks before and 6 weeks after surgery. This includes cigarettes, cigars, vape with nicotine etc. This will reduce the risk of
Thrombosis (DVT and PE),
The risk of infection by 2.04 times
The risk of nonunion by 2.5 times (5)
Use Vit D (1000IU) and Calcium (500mg) supplement 6 weeks prior and 6 weeks after the surgery.
Use high dose Vit C (500-1000mg) 6weeks before and 6 weeks after the surgery This will reduce the risk of CRPS.
Dont use Non steroidal anti-inflammatory drugs NSAIDs Before and 6 weeks after surgery.
On the day of surgery
Dont eat 8 hr before surgery
You can drink clear water up to 3hr prior to surgery
Take your medication that you use regularly on the morning of surgery.


Treatment with 4th generation Metatarsal Extraarticular Transverse & Akin META Osteotomy
Insertional Achilles tendinopathy
What is Insertional Achilles Tendinopathy and Haglund's deformity?
Insertional Achilles tendinopathy and Haglund’s deformity is a condition affecting the rear part of the heel bone, presenting with a painful thickening of the lowest part of the Achilles tendon, a sore lump, difficulty wearing shoes and performing physical activities.
How does Insertional Achilles tendinopathy and Haglund’s deformity develop? (Išskleidžiamas)
It is now believed that with longer upper end of the heel bone, the contact between upper rear corner and the insertional part of the tendon is causing repetitive micro damage. In the long run degeneration develops:
Tendinopathy - Achilles tendon becomes thickened and painful secondary to fat, abnormal collagen, calcium, new vessels and nerves deposits.
Haglund’s deformity - The bone spur progressively enlarges at the rear upper end of the heel bone.
Retrocalcaneal Enthesofite - additional spur forms behind Achilles tendon insertion point.
Retrocalcaneal bursitis - inflammation of the fluid sack between the Achilles tendon and the heel bone.
The complex of all these changes is called Haglund’s syndrome. The patient complains of the painful lump, difficulty finding appropriate shoe-wear, resuming physical activities.
Non Operative treatment (išskleidžiamas)
Non operative treatment is limited and often provides only temporary relief.
Pain killers, icing, activity modification often provides only temporary relief
Physiotherapy with Excentric strengthening protocols is effective in up to 30% (1).
Silicone heel cups may relieve symptoms temporarily, but will shorten Achilles tendon and worsen the process in the long run.
Appropriate shoe-wear with soft heel cup or slippers, prevent painful rubbing.
Extracorporeal shock wave therapy is more effective for the treatment of Non insertional Achilles tendinopathy. (2)
Ultrasound guided Steroid injection can increase the risk of tendon rupture.
PRP - Platelet Rich Plasma injection effectiveness for IAT or NIAT is not proven. (3)
Operative treatment
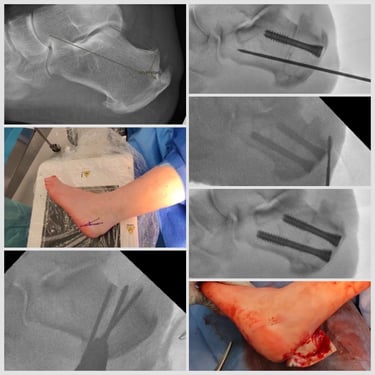
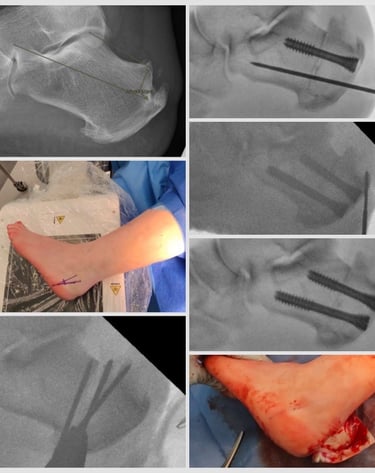
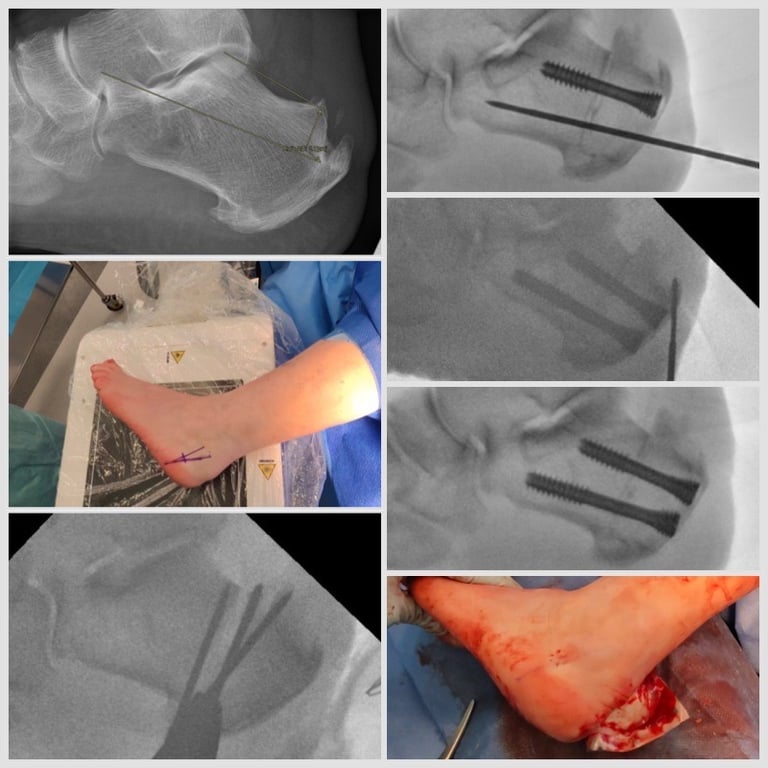
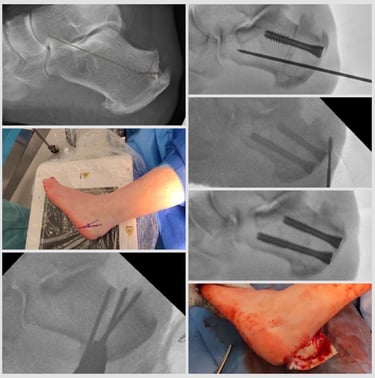
Mr. Donatas Chlebinskas offers percutaneous Zadek Dorsal Closing Wedge Calcaneal Osteotomy (DCWCO) for the management of IAT. Procedure is performed on the day surgery basis, usually under general anaesthetic. Percutaneous 4-6mm incisions are used. Bone cuts are performed under x-ray control using slow spinning high torque Shannon burrs and Wedge burrs. The wedge of bone is taken out based at the top of the rear heel bone. Once closed and fixed rigidly with special screws - fixation is strong
enough o permit weight bearing from day one, but back slab is applied and non weight bearing regime is advised for first 2 weeks. This operation assures the following affects:
Haglund deformity bone spur is moved away from the achilles tendon, decreasing the impingement.
Achilles tendon insertion point is raised higher therefore decreasing the tension on the tendon.
Rarely the operation can be combined with rear ankle keyhole procedure called posterior ankle arthroscopy to remove the retrocalcaneal bursa and shave the remaining bone spur.
Why should you choose percutaneous Zadek osteotomy over standard open procedure?
Small percutaneous incisions reduces the risk of infection and wound complications, which is quite high in open surgeries because of poor blood supply to the region.
Zadek osteotomy does not involve detaching and reattaching Achilles tendon as the standard open surgery. Therefore Achilles tendon rupture risk is reduced.
Less postoperative pain. Lower analgesic requirements.
Ankle is kept in neutral rather than en pointe position and weight bearing is permitted 2 weeks after surgery as pain allows.
Lowe risk of Thrombosis as DVT and PE.
This surgery is suitable for profesional athlets and permits return to competitive athletic activities at 21 weeks in open surgery. (3) This will be reduced by percutaneous procedure.
What is the post operative regime for the best outcomes:
2 weeks using a Back slab.
2 weeks elevation at the heart level 23hr a day.
At 2 weeks follow up appointment the wound check is performed.
At 2 weeks follow up appointment waking boot is applied and weight bearing is permitted as pain allows. Usually waling with two crutches for 2 weeks and one crutch in the opposite hand for further two weeks is required.
At 6 weeks follow up appointment X-Rays are obtained.
At 6 weeks appointment regular comfortable footwear is commenced.
From 6 weeks after surgery gradual return to physical activities are advised. Starting with walking, cycling, swimming, transitioning to jogging at 10-12 weeks after surgery.
It is not recommended to drive a car 6 weeks after surgery. (You can drive automatic gear box car 2 weeks after surgery if your left foot was operated).
Possible risks and complications:
Intraoperative
Nerve or vessel damage (numbness pins and needles or bleeding, necrosis)
Achilles tendon damage
Incomplete resolution of the lump
Calcaneocuboid joint damage
Anaesthetic risks
Early postoperative
Swelling, bruising, pain
Surgical site infection (superficial wound infection or osteomyelitis)
Thrombosis (DVT and/or PE)
Late postoperative
Plantar fasciopathy - pain at the bottom of the heel
Recurrence (deformity comes back).
Nonunion (bone cut doesn’t heal) Pseudoartozė (Kaulinis nesugijimas),
Maluinion (bone heals in undesired position)
Hypertrophy of the scar (sensitive big scar).
Complex regional pain syndrome (Sensitive, swollen, atrophic foot) 0,4%
Metalwork failure (screws break, migrate, or irritate tissues)
Need for further surgery.
List is extensive but likelihood of these risks is extremely small. Most of them only theoretical and not reported in the literature.
How to prepare for the surgery
Preoperative period
Have WEIGHT BEARING x-ray radiograms. Lateral of the foot and ankle and AP of the ankle and dorsoplantar view of the foot.
MRI scan is not mandatory, but helps to better plan surgery and differentiate from other potential problems that may present with similar symptoms.
Blood tests including Full Blood Count, Coagulation screen, Urea & Electrolytes, VitD not older than 1 month;
Tell the doctor if you have diabetes and if so have HbA1c not older than 1 month.
Tell the doctor if you are using blood thinning medication
You can use Aspirin throughout the procedure for cardiological reasons.
Don’t use nicotine 6 weeks before and 6 weeks after surgery. This includes cigarettes, cigars, vape with nicotine etc. This will reduce the risk of
Thrombosis (DVT and PE),
The risk of infection by 2.04 times
The risk of nonunion by 2.5 times
Use Vit D (1000IU) and Calcium (500mg) supplement 6 weeks prior and 6 weeks after the surgery.
Use high dose Vit C (500-1000mg) 6weeks before and 6 weeks after the surgery This will reduce the risk of CRPS.
Dont use Non steroidal anti-inflammatory drugs NSAIDs Before and 6 weeks after surgery.
On the day of surgery
Dont eat 8 hr before surgery
You can drink clear water up to 3hr prior to surgery
Take your medication that you use regularly on the morning of surgery.
Treatment with Zadek osteotomy

Chronic Ankle Instability
What is Chronic Ankle Instability?
Chronic Ankle Instability is a condition that may develop after an ankle sprain, resulting in ruptured ligaments on the outer side of the ankle. Most patients recover from an ankle sprain by simple measures as icing, analgesics, bracing, physiotherapy and gradual return to physical activities. However up to 20-40% of patients may continue to experience symptoms of ankle instability such as giving way, insecurity playing sports, pain or locking. Untreated instability may lead to inflammation inside the ankle joint called synovitis, further cartilage damage, bone spurs ultimately leading to arthritis. In case of unsuccessful non operative treatment it is worth seeing an orthopaedic surgeon, where following a history taking, clinical exam and investigation review, discussion can be carried out about operative treatment.
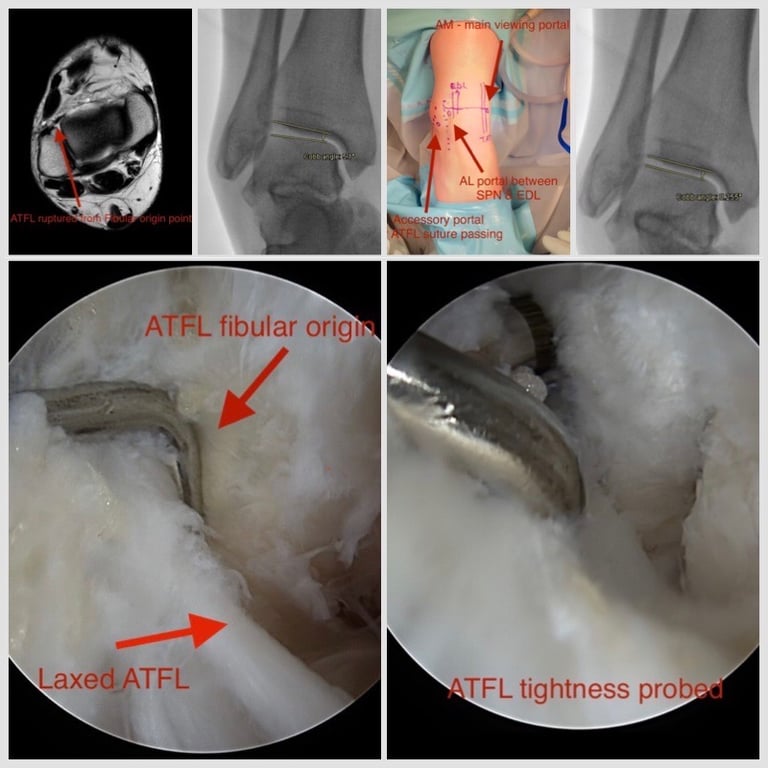
What does the All Inside Brostrom operation entail?
Operation can be carried out under a regional block, general or spinal anaesthetic. First the ankle is examined under x-ray guidance to asses the instability. Thereafter, via small incisions a camera called arthroscope along with other instrument is introduced to the joint to assess and address the changes. After any cartilage defects or bone spurs impeding free movement of the joint were addressed, All inside Brostrom ligament repair is performed. Often lengthened and loose ligament on the outer side of the ankle called ATFL is sutured tightening it and reinforced with fibre tape augment called internal brace.